AIMS Journal, 2024, Vol 36, No 1
Editor’s note: In this quite shocking account of disrespect and neglect, Grace describes the arrival of her first baby. With Grace’s permission, the section that explains what actually happened at the hour of his birth is written in my words. This is because, for Grace, the emotions attached to this time are so complex, and her memory of the trauma so detailed, there weren’t enough words, or a way of putting them together, that made sense. In fact, what happened was senseless. Not all of her care felt bad though. Her good experiences came from being listened to with respect and trust by practitioners with whom she had built a relationship. If her care had been like this throughout her time in hospital, Grace would have had a very different story to tell.

By Grace Hall
Our story starts as first-time parents, full of dreams and preparations for our firstborn’s arrival, informing my GP that I was pregnant and really looking forward to the journey. We did much planning and preparation for this magical moment in our lives. I had the majority of the offered screening tests done, saw complementary therapists and followed the suggested guidelines.
I was offered a test for gestational diabetes (GD) due to my apparent ethnicity, and was referred to a consultant despite results being normal, and despite me being very healthy and classed as low risk. The referral was useful however, as I developed pelvic girdle pain later on in pregnancy and the consultant obstetrician was very supportive. He provided me with ideas on how to relieve the discomfort and further explanations on how to have a positive pregnancy and labour experience. He helped me create a birth/care plan based on my preferences, explained how to cope with pregnancy and labour discomforts, and made recommendations for a comfortable labour. I saw the same consultant, who was at the time the Head of Obstetrics at my local hospital, three times through pregnancy and I felt that the continuity of care was reassuring and a positive experience.
When I first went into hospital, after labour started, I saw several different midwives and, after being sent home once for not being in active labour, we returned to the hospital and I was examined, and offered a side room in which to rest – and there I stayed for the next 14 hours. During this time I was given a dose of pethidine, but otherwise was without any assistance. I felt secure being in a place I could call midwives anytime if I felt unwell, however my labour slowed down and I was finally able to sleep.[1] During my awake intervals I ate the food and drank the water I brought in my suitcase and I used hypnobirthing to cope with the pain.
What I did not realise at the time, was that the absence of anyone to check on me after strong pharmacological medication was administered, or even to provide me with food and water, was the start of neglect and a pattern that set the unsafe scene of malignant neglect that almost led to my baby and I not surviving labour and birth. There were systematic errors, broken communication between staff, and all the recommendations made by my consultant obstetrician were disregarded and written off with drastic and long-lasting consequences for both my son and me.
This is what happened: After 14 unsupported hours of labour in a sideroom, a midwife finally came at the very end of her shift and offered a vaginal examination to assess whether Grace’s cervix was opening. The midwife apologised and said that she was only 2cm dilated. Grace accepted this and got up to walk about. Only a little while later she felt the need to push and told the midwife. The new midwife responsible for Grace’s care said that she could not possibly be ready yet and that she could not perform another vaginal examination so soon after the previous one. Grace insisted on an examination and sure enough, in under one hour she had dilated to 8 cm. At this point she was admitted to the labour ward. The midwife on the labour ward appeared fed up and unwelcoming. She tutted and sighed and told Grace that it would be another three hours before her baby was born. Grace then started ‘vocalising’ (making the sort of noises that women make as they are about to give birth) and the midwife told her (in what felt like an unsupportive tone) not to scream as it was a waste of her energy and wouldn’t change anything. Grace’s original plan for a waterbirth had already been changed, and now she had her request for an epidural declined. She remembers that no attempt to comfort her physically or emotionally was offered instead. Very quickly Grace felt ready to give birth and asked to be examined again. The midwife asked her to lie on the bed but instead of examining her applied a belt monitor and started asking detailed questions about her name and address - even though it was clear that Grace could not speak at this point. Unable to manage the contractions in this position, Grace tore off the monitor and stood up by the bed. A student midwife asked permission to remove Grace’s underwear and a quick look showed a bulging bag of membranes clearly visible at the introitus (entrance to the vagina), a sign that the birth was imminent. Instantly, the membranes ruptured covering the student midwife and going into her eyes so that she could not see properly for a moment. A pillow was quickly placed at Grace's feet, but it was not enough. Her baby followed so quickly that Grace did not have time to catch him herself.[2] He shot head first onto the floor and slid under the bed yanking on the still attached placenta and snapping the cord. This resulted in a very shocked baby (otherwise unharmed), a very heavy bleed for Grace, and a sense of trauma that she carries to this day.
After the birth I was so confused, in shock. My body started to somatise[3] the experience and the midwife made a referral for me to be seen by my GP. The meeting with my GP was generously paced and welcoming and he was able to hold the space for me in a way I had not yet felt or seen since the birth of my child. He was appalled with my birth story and helped me identify several failures in the care we received, issues that I had previously attributed responsibility for to myself. My GP kindly wrote a letter to the Head of Obstetrics to ask for his assistance with a Birth Reflections session and in addressing the negligence.
My GP letter initiated our process of complaint. He was able to articulate the failures from the physician’s point of view. He described how I felt, my medical history and how the event was impacting me at that moment. This felt very positive. Being my GP, he already had an idea of who I was, he knew my husband and our family, and he was able to paint a picture of how much the events leading to the birth of my child had affected me.
The consultant obstetrician promptly responded and invited us for a meeting to hear from me about my concerns and grievances, and to try and explain how so many mistakes, that led us to feeling unsafe, scared and scarred, had happened. We attended the meeting at his office in the hospital. He was kind and warm with great listening ability. He held space for us while he explained how the events reflected an unacceptable standard of care. He said that there were several midwifery errors and that he fully supported our formal complaint with PALs (patient liaison services). The consultant also recommended that my labour and son’s birth records were reviewed by us in this meeting; however the documentation was not available, so he recommended that we return when he had all the records with him. We were made aware that legally we had the right to copies of my record and to review the documentation with a clinician. So we requested it and agreed to return to discuss it.
Unfortunately, the warm and caring atmosphere of the previous meeting with my obstetrician was not repeated at the following meeting we attended at the hospital. We had a consultant midwife and the Head of Grievances join the meeting. She was extremely formal, cold, and defensive. She used very harsh language with us and, while she had our records with her, they were missing the page recording the time period in which the negligence at the birth of my son happened. She also mentioned that many of their procedures had changed since we gave birth at the hospital (only a few months prior to this meeting) and that the changes were unrelated to what happened to me - despite the fact that she had heard what happened on the night of the horrific events of my son’s birth, as she was on duty at the time.
This was so heartbreaking to hear and face as we hoped that by reading the records we could make sense of what happened. But this was not possible. I felt even more lost and broken inside to see that what happened to my son was not worth one single acknowledgement from the midwife responsible for grievances. Midwives are professionals supposedly responsible for supporting women emotionally during one of the most crucial life changing events in their life. My husband even cheered to hear that some of the procedures had changed, believing that it was due to our near-death experience. However, as mentioned previously, the consultant midwife took pains to say that these changes were unrelated to events that occurred at the birth of our baby, which felt like continued gaslighting - so much so that the consultant obstetrician asked for the meeting to come to an end until further investigation was carried out to discover what had happened to the missing page in my records.
I believe this doctor put a stop to the meeting as a compassionate gesture because he could see how the consultant’s midwife’s cruel indifference, and her defensive way of using legal terminology and detached jargon, was affecting us - especially so recently after the experience that would mark us for the rest of our lives. Once the consultant midwife left the room, the consultant obstetrician was very empathic and said to us that this was such a tragic and embarrassing incident, and that further investigation would be done to find my missing records. The doctor said to us that we could continue to bring our grievances forward and beyond the NHS.[4] However, he questioned whether this was something we would be able to cope with or wish to do for the next few months and probably years while the whole case went further. He graciously explained to us that continuing with the grievances would be like a dark shadow of a cloud over our heads accompanying us wherever we went, preventing us from enjoying our son who was alive despite all the occurrences. The consultant obstetrician then said that many couples who come to see him with lesser complaints, and who sit in the very same seats as we were sitting, did not have the opportunity to hold an alive baby in their arms.
We walked away feeling very reflectful, grateful for our lives, looking forward to meeting again to understand what happened to my records and to having some sort of closure. Months after this meeting, we were contacted once again by the obstetrician and informed that a part of my records was still missing. He asked if we would like to come in and discuss next steps. We decided against it. Despite his very strong remark about other parents who had fatal outcomes for their babies, we appreciate that my obstetrician’s intentions appeared to be good.
In hindsight, was his gentleness and supportive ways a tactic of “good cop, bad cop”? We will never know.
The only thing we know is that being listened to, acknowledged and validated made us feel held enough to move on, at that time.
What is my take from experiencing the complaints and debriefs processes first hand? It is that it can be extremely draining. It can be very upsetting to have to review and learn from the information recorded (if they have not lost it) as it is often in medical jargon and comes from a different perspective than the parents’ experience. Sometimes the notes are written in a way that makes it sound as if the events were a failure or incapability of the mother. It can be extremely hard to relive the labour story and accept that the things that could and should have been done did not occur. However, there are some people who have found the experience an aid to their healing process. I work with birthing families every day and I see all situations in the birthing rooms (at home, in ambulances, birthing centres, labour wards or theatre) and some of the families I have worked with have found consolation, validation and understanding from the process of a birth debrief with their Trust and facilitation through PALs.
The main thing I would love is for families to set their expectation at the right level when deciding to pursue a complaints process, as, in my observation, NHS members of staff will rarely admit error if their admittance will lead to a court case being lost. Nevertheless, parents may find closure to their stories and be able to restart their journey with a better understanding for next time.
So, please do not think that making a formal complaint is a useless exercise, or something to fear. Women who feel broken, guilty, let down and unable to cope with caring for themselves and their families, should not have to suffer in silence. It is your midwife and doctor’s moral, ethical and legal duty to provide safe and dignified care to you and your baby. Making a complaint can be very beneficial both for your recovery process and for highlighting your concerns about the standard of care provided by the professionals that may be letting you and the system down.
The journey has not been easy, however, being able to express my truth in safe places, and being supported through the process, enabled me to transcend the pain to a place where, after some years, I was able to reframe my experience and give birth to my second baby at home, calmly, respectfully and well supported by those that I love.
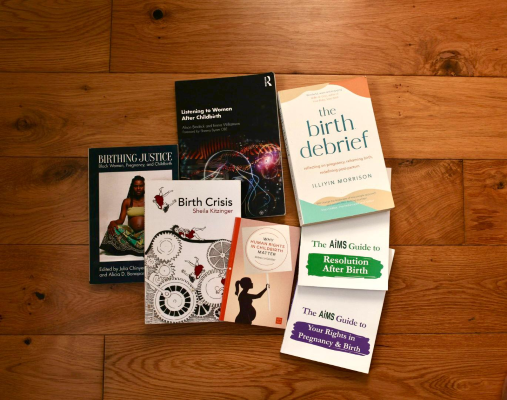
Grace’s useful reading list
Birth Crisis by Sheila Kitzinger - ASIN: B000OI18QI
The AIMS Guide to Resolution After Birth - ASIN: B086T266KQ
The AIMS Guide to Your Rights in Pregnancy and Birth - ASIN: B08SWTVFMJ
The Birth Debrief by Illiyin Morrison - ASIN: B09DK3MYJ9
Listening to Women after Childbirth by Alison Brodrick - ASIN: B084PY476Q
Why Human Rights in Childbirth Matter by Rebecca Schiller - ASIN: B01LYGNL1J
Birthing Justice edited by Alicia D. Bonaparte and Julia Chinyere Oparah - ASIN: B0BX9HTYKB
Author Bio: Grace Hall is a mother, Hypnobirthing educator, holistic doula, complementary therapist and ceremonialist, supporting women to reclaim their autonomy as they enter motherhood. Grace believes that she has inherited her deep calling to this work from her paternal grandmother and great grandmother, both of whom were traditional midwives in Brazil.
[1] Pethidine will slow labour in the early stages and it also acts as a powerful sedative.
[2] Editor’s note: Had Grace been given empathic support and not disturbed by the opinions and moods of others, her own perception and instincts might well have guided her to move closer to the floor where she could have received her baby safely into her own hands. This powerful instinct is completely disrupted when other people tell you what to do and when they suggest that you cannot trust what you are feeling in your own body. A note to anyone who is with a woman in labour: Listen to the mother, believe her and support her.
[3] Editor’s note: Somatise means to manifest (psychological distress) through physical symptoms.
[4] Editor’s note: When the outcome of a person’s complaint is unsatisfactory, they can take it to the ombudsman.
The AIMS Journal spearheads discussions about change and development in the maternity services..
AIMS Journal articles on the website go back to 1960, offering an important historical record of maternity issues over the past 60 years. Please check the date of the article because the situation that it discusses may have changed since it was published. We are also very aware that the language used in many articles may not be the language that AIMS would use today.
To contact the editors, please email: journal@aims.org.uk
We make the AIMS Journal freely available so that as many people as possible can benefit from the articles. If you found this article interesting please consider supporting us by becoming an AIMS member or making a donation. We are a small charity that accepts no commercial sponsorship, in order to preserve our reputation for providing impartial, evidence-based information. You can make donations at Peoples Fundraising. To become an AIMS member or join our mailing list see Join AIMS
AIMS supports all maternity service users to navigate the system as it exists, and campaigns for a system which truly meets the needs of all.